Introduction
Following the recommendations set out in the Rethinking Schizophrenia Care Pathway in Europe study paper, the next phase of the project — Country Profiles: Beyond Mental Health – A Brain Health Approach to Schizophrenia Prevention and Care — will focus on an in-depth analysis of country-specific models of care. After a roundtable meeting in Poland on 5 June 2025, we are now moving forward with Denmark. On 8 December 2025, the European Brain Council (EBC) and the Danish Psychiatric Association together with the Danish Brain Council organised a webinar titled "A Comprehensive, High-Quality Approach to the Treatment of Schizophrenia in Adolescents and Young Adults". This webinar gathered key stakeholders from healthcare, social, education, employment, research and patient organisations. The event provided an opportunity to hear perspectives that combine evidence and life experience but also to discuss innovative strategies for improved schizophrenia prevention and care in Denmark, within a broader European brain health framework.
Key Takeaways
- Strong early-intervention infrastructure but capacity gaps remain. Denmark has nationwide OPUS early-intervention services with evidence of improved symptoms, functioning and cost-effectiveness, yet teams cover only ~70% of incident cases and there is a marked drop in service intensity after two years.
- Major unmet needs in psychosocial functioning, comorbidities and physical health. People with schizophrenia face low psychosocial functioning, cognitive impairment, substance use, homelessness and excess mortality, and they receive poorer quality somatic care than people without schizophrenia.
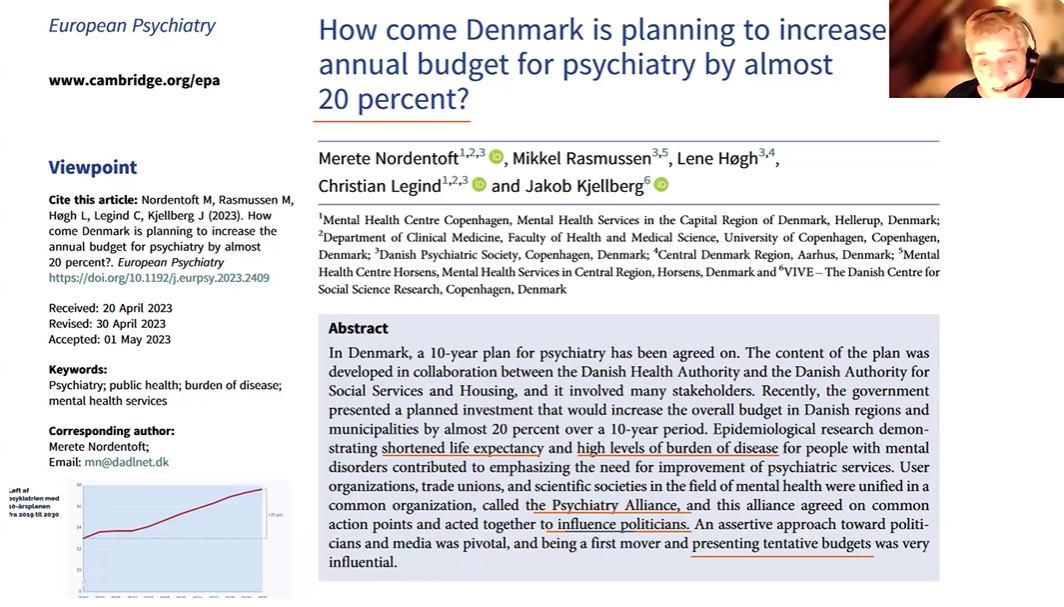
- Ambitious 10-year national plan and major funding increase. Denmark has agreed a cross-party, 10-year psychiatry plan with mental health spending at ~6.8% of the health budget, aiming for parity of quality with cancer care and focusing on access, coordination, equity, research and anti-stigma efforts.
- Comprehensive, life-course and community-oriented service mix. The system combines early-intervention teams, flexible assertive community treatment, individual supported employment, Housing First, supported accommodation, acute outreach, caregiver psychoeducation and preventive initiatives such as headspace (a youth mental health service offering free and anonymous counselling to young people aged 12–25) and high-risk family studies.
- Brain-health and European leadership perspective. Denmark explicitly frames schizophrenia policy within a broader brain-health agenda and, as EU Council Presidency holder in the second semester of 2025, positions its coordinated, data-driven model of schizophrenia care as a reference point for European mental- and brain-health policy dialogue.
Welcome & Opening Remarks
The webinar was opened by Prof. Suzanne Dickson, President, European Brain Council, Prof. Morten Lorenzen, Vice Chair, Danish Brain Council and Dr Jennifer Hall, Technical Officer – Mental Health, WHO Athens Quality of Care Office & WHO EURO Mental Health Flagship. Suzanne highlighted that the webinar aims to present Denmark Country Profile-specific findings and youth-focused policy recommendations to improve comprehensive, high-quality schizophrenia care through early detection, access to innovative pharmacological and psychosocial treatments, integrated models and digital tools within a brain-health, biopsychosocial framework. Morten referred to a recent Lancet study 1 and highlighted recent figures on the occurrence, mortality, and economic burden of brain disorders in Denmark. They stressed the urgent need—both in Denmark and across Europe—for coordinated, science-based approaches to brain disorders, with strong early intervention, research, patient and family involvement, and better translation of evidence into practice and policy.
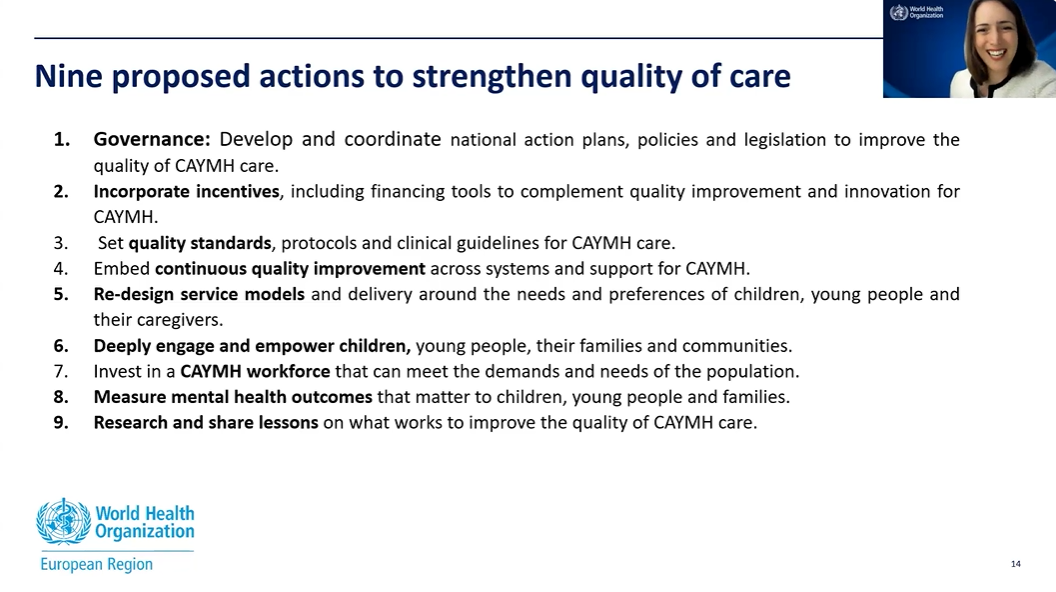
Dr Jennifer Hall presented the new WHO report “Child and Youth Mental health in the WHO European Region”. Jennifer explained that WHO data show a sharply rising prevalence of mental health conditions among children and adolescents in the region—especially anxiety in 15–19-year-olds—alongside persistently high suicide as a leading cause of death and a very uneven, overall insufficient service response, with major gaps in policies, community-based services, school provision and workforce capacity. She then outlined nine co-developed actions to strengthen quality of care, centred on stronger governance and multisectoral plans, quality standards and continuous improvement, innovative and co-designed service models, meaningful participation of young people and families, workforce development, and better data and research—highlighting clear synergies with the Rethinking Schizophrenia project.
Keynote Address 1: The Rethinking Schizophrenia Project
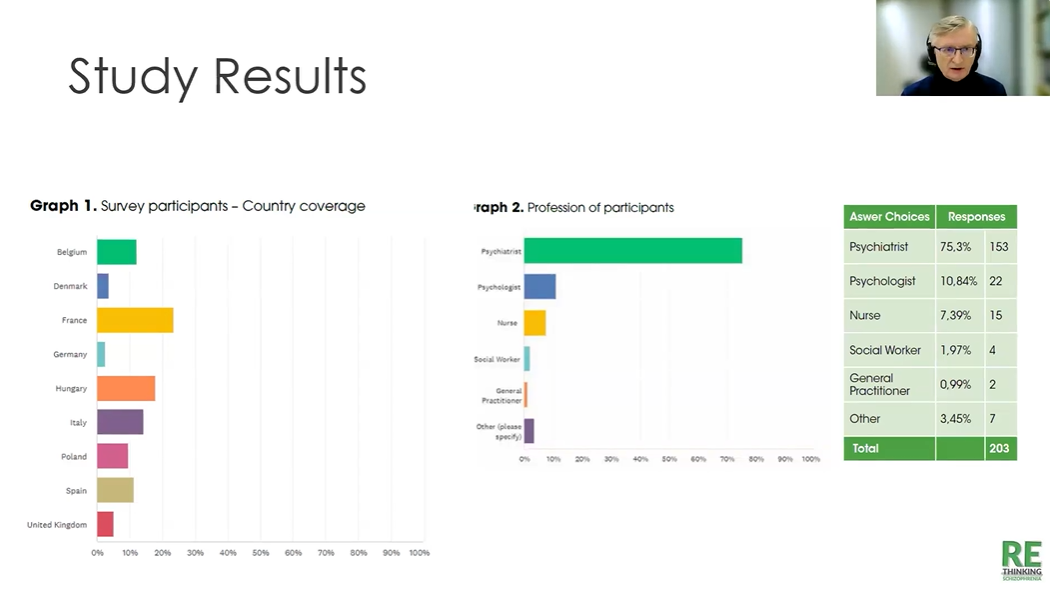
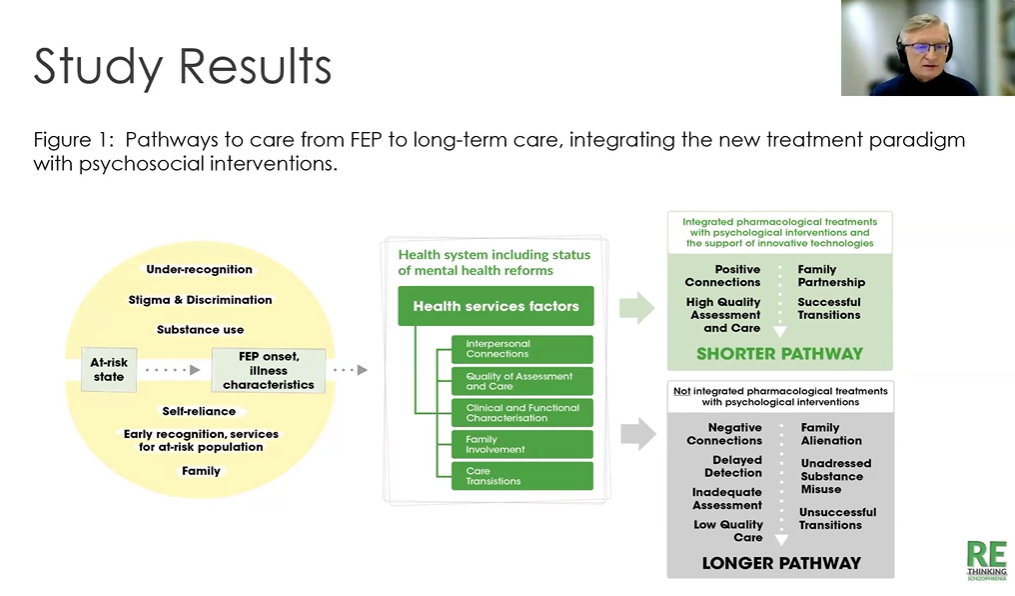
The first keynote presentation set the scene of the webinar. Prof. Pavel Mohr, National Institute of Mental Health, Prague presented the Phase II “Rethinking Schizophrenia” study, which surveyed over 200 mostly experienced mental health professionals in nine European countries to map youth psychosis care pathways and found major gaps: limited access to early detection and early intervention services, discontinuity of care, fragmented outpatient follow-up, and persistent stigma despite existing anti-stigma initiatives. Based on the results and the data, a clinal model was designed “Pathways to care from FEP to long-term care, integrating the new treatment paradigm with psychosocial interventions and the support of innovative technologies”. Pavel Mohr indicated that duration of untreated psychosis is an important predictor for a long-term outcome. This is also part of the Rethinking Schizophrenia initiative aiming to reduce duration of untreated illness. He explained that the project produced eight key recommendations, including scaling early psychosis programmes, ensuring equitable access to innovative pharmacological and psychosocial treatments, strengthening coordinated multidisciplinary and recovery-oriented care, addressing physical health and social determinants, building workforce capacity, and promoting data-driven, research-informed policy and practice. A paper with the results of the survey was just submitted for publication.
“By adopting a biopsychosocial approach and integrating brain health into national policies, we can shift the paradigm in schizophrenia care.”
“Our role is to bridge these worlds so that insights from science are translated into practice and patient experiences inform clinical decisions and political strategies.”
“We are seeing a sharp rise in mental health conditions among children and adolescents across the region, while the response remains highly variable and, in many places, insufficient—there are still major gaps in policies, community services, school-based support and workforce capacity.”
Keynote Address 2: Schizophrenia Care Pathways in Denmark
Prof. Merete Nordentoft, Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark presented a brief version of the Rethinking Schizophrenia Country Profile for Denmark. Merete explained that Denmark is in a unique position because all political parties agreed on a historic psychiatry investment—around a 35% budget increase—built on strong epidemiological evidence of high mental-illness burden, coordinated advocacy through the "psychiatry alliance," and a clear national plan with 37 recommendations. She highlighted that Denmark already has nationwide early intervention services (OPUS), FACT teams and specialised outreach, with robust trial and health-economic data showing that early psychosis intervention is clinically effective, reduces hospitalisation and mortality, and is overall cheaper and better for young people. She also presented other key pillars of the new plan, including scaling IPS supported employment, Housing First for homeless people, a 24/7 professional helpline and psychiatric emergency outreach, positioning the Danish model as a potential inspiration for other countries. The Country Profile for Denmark will be released soon.
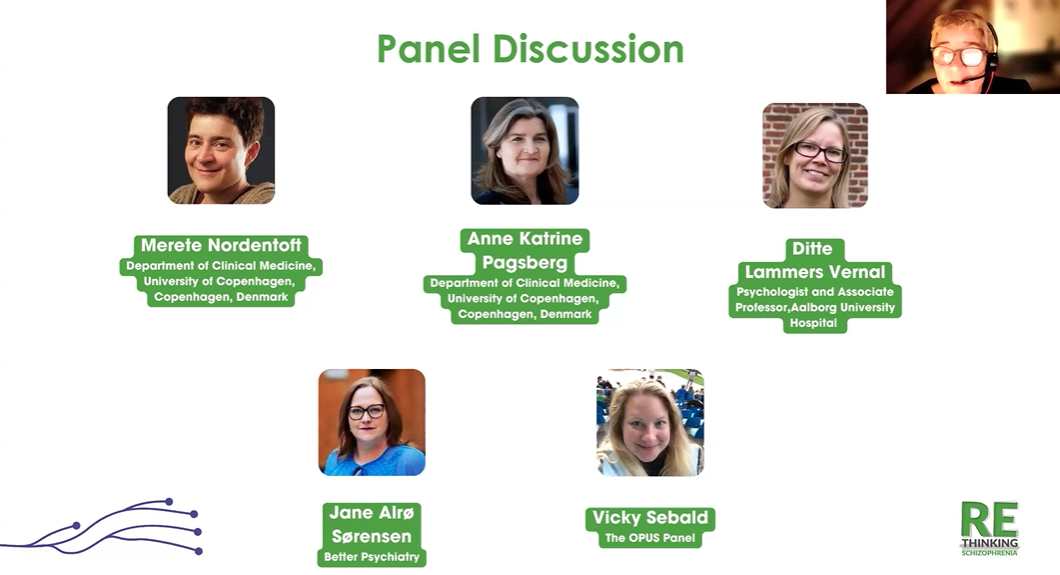
Panel Discussion
Merete moderated a panel consisting of Vicky Sebald from the Opus panel, giving the patient perspective to all this, Prof. Anna-Katrine Pagsberg from the Child and at Adolescent Psychiatry and Didi Lamas-Vernal, Psychologist and Associate Professor. Unfortunately, Merete excused Jane Alroe-Soerensen from the patient organization Better Psychiatry.
Anne-Kathrine Pagsberg stressed that one of the most serious gaps is the transition at age 18 from child and adolescent to adult services, which often disrupts continuity of care, and she highlighted ongoing efforts to develop youth-focused early intervention models similar to OPUS and to improve European collaboration on psychopharmacology and innovative treatments (e.g. TMS, a brain-stimulation treatment that doesn’t require surgery, and that might offer an alternative or complement to medication for some patients) for young people. Vicky Sebald, speaking from lived experience, emphasised diagnostic delays, the gap between intensive OPUS care and standard adult services, and the challenge of building trust in psychiatry for people with schizophrenia, while warmly welcoming youth-tailored, digital and peer-based supports (VR tools, apps, online groups) that make care more accessible and relatable. Ditte Lammers Vernal underlined the huge mortality gap and insufficient attention to physical health in schizophrenia, called for broader access to evidence-based psychotherapies (including VR-based voice dialogue) and expressed pride in OPUS and the integration of peer workers, while warning that workforce shortages and pressure must not crowd out research, education and a sustainable work environment.
Merete Nordentoft highlighted the strengths of the Danish system—OPUS, the Opus panel for destigmatisation, a tax-financed healthcare system and national quality registries—and welcomed the 10-year psychiatry plan’s focus on dual diagnosis, homeless and marginalized groups, excess mortality reduction and recovery, while recognizing that restoring trust (among patients, families and professionals) remains crucial. Suzanne Dickson added a European perspective, warning about the lack of innovation and access to new brain medicines in Europe compared with cancer, and called for stronger lobbying, research funding and regulatory action, to which Merete responded by agreeing on the need for better psychotropic drugs and stricter, evidence-based standards for managing side effects and improving psychopharmacological care.
The panel was followed by a questions and answers session during which Suzanne Dickson argued that the very broad use of the term mental health disorders—from mild anxiety to severe illnesses—risks overstretching already limited psychiatric resources and obscuring the fact that conditions like schizophrenia are major brain disorders that require intensive, specialized care. Pavel Mohr agreed and linked this to the emerging brain health agenda, explaining that psychiatry and neurology jointly need to refocus on brain disorders themselves, while learning from countries like Denmark that have secured substantial investment and built comprehensive early-intervention systems. Merete Nordentoft finally emphasised the high burden and economic cost of schizophrenia (including large losses in working years), noting that, in Denmark, disorders such as schizophrenia, depression and anxiety rank among the top contributors to disease burden and productivity loss, though exact figures will vary by country and context.
“In Denmark we’ve managed to build nationwide early intervention services like OPUS, flexible assertive community teams and now a 10-year psychiatry plan with a 35% budget increase—together, these are major steps toward truly comprehensive care for people with schizophrenia.”
“People with severe mental illnesses need complex care: not just pharmacotherapy but also psychological, psychosocial and social support services across the whole pathway.”
“OPUS was fantastic for me, but going from that intensive support to ‘normal’ treatment felt like being dropped—some people simply aren’t ready for such a big step down in care.”
Concluding Words
Suzanne Dickson concluded that the webinar had clearly shown both the urgency and the opportunity in youth-focused schizophrenia care: WHO data point to rising mental health needs in young people, while the Rethinking Schizophrenia project and the Danish experience highlight strong evidence for early detection, integrated care pathways, innovative treatments (including digital tools and TMS), and programmes like OPUS that improve outcomes and can even reduce costs. She stressed key gaps such as the transition from child to adult services, the 15-year mortality gap, limited access to effective pharmacotherapies, and called for a paradigm shift in schizophrenia care, backed by stronger advocacy, research and regulatory action in Europe.
Vinciane Quoidbach, Research Project Manager, European Brain Council closed by explaining that the country profiles (Poland, Denmark, next Germany) serve as a “reality check” to confront survey data with on-the-ground systems, showing the urgent need for upstream, personalised, biopsychosocial care pathways, cross-sector coordination, and policies that embed brain health in national strategies. She underscored that a multi-stakeholder, brain-health–oriented approach is essential to drive systemic reform in schizophrenia care, and while thanking all the speakers and participants, outlined next steps: the next webinar that will take place on 4 March 2026, presentations at major congresses, and the forthcoming scientific publication (European Journal of Psychiatry).
“The transition from child and adolescent services to adult psychiatry around age 18 can be a major barrier to staying in treatment.”
“The country profiles aim to create momentum for systemic reform by embedding brain health in policy and strengthening personalised, cross-sector care pathways for young people.”
“Patients with schizophrenia on average die around 15 years earlier than people without mental disorders; we need much better care for their physical health.”